Brand Surveys and Testing

Aug
Nursing Homes Close as Need for Care Grows
jerry9789 0 comments Brand Surveys and Testing, Brandview World
Nursing Home Challenges
According to a report by the American Health Care Association and National Center for Assisted Living (AHCA/NCAL) in April 2022, more than 1,000 nursing homes have closed since 2015. This breaks down to 776 closures before the COVID-19 pandemic and 327 closures during the pandemic.
The same report also projected 400 nursing homes to close in 2022 based on financials at the time. While the Centers for Medicare & Medicaid Services reported 135 nursing homes closing in 2022, it is believed the number could be higher. This is due to possible discrepancies between the time a closure plan is submitted by a facility and its full execution to be listed in the federal database.
Staffing shortages and low reimbursement have long been recognized as factors for nursing home closures even before the pandemic. Rising wages and increased operation and maintenance costs in recent years exacerbated the situation, especially in rural areas.
The Impact of Nursing Home Closings
These closures resulted in former residents transferring to another facility, which in most cases, was farther from home. Some even must move twice after the first nursing home they transferred to subsequently closed. The process could also take weeks as social workers look for placements so a patient might find themself staying in a hospital in the meantime. Conversely, some nursing care facilities are keeping beds vacant because they don’t have enough workers.
Amidst these challenges, the need for long-term care grows with baby boomers joining this group.
Nursing Home Alternatives
While the pandemic put a spotlight on the difficulties faced by the nursing care industry, it also opens opportunities for reforming and improving nursing homes. It also paves the way for exploring nursing home alternatives, such as in-home care for seniors. However, home care may prove to be the more expensive option and while it offers more personal and tailored assistance, you might have a senior who prefers or thrives more in a group setting like the one offered by assisted living communities.
Then there are group homes and family-style nursing homes, which are both small-scale options for assisted living. While a typical nursing home holds over 100 resident beds on average, a group home can house between five to 10 people (or 20, depending on the state) while family-style homes host 10 to beds. These setups allow for more personalized care and a higher staff-to-client ratio in a sociable, homelike setting with home-cooked meals.
Due to being smaller in scale and not as advertised as regular nursing facilities, most group homes might slip past the radar of older adults or their loved ones seeking assisted living. With well-developed branding, however, smaller-scale assisted living communities can stand out even from the shadows of larger facilities and get their message across better to the seniors most suited for the living arrangements they offer.
MDSA can help you develop your branding, thanks to an array of services such as Brand Development Research and Segmentation Studies backed by over three decades of experience. Whether you are a smaller residential care home trying to get the word out or a larger assisted living community looking to reach the ideal senior or even the skilled nurses you need, we can help you find the right market research solution for your branding needs.

Apr
How healthcare people can help underserved populations
jerry9789 0 comments Brand Surveys and Testing, Brandview World, Burning Questions
There’s no shortage of knowledge about the healthcare needs of underserved communities in the US such as the Hispanic, Black, American Indian/Alaska Native, and Native Hawaiian/Pacific Islander subpopulations. What may be lacking are workable and effective efforts to address these needs.
There are two main parts of this problem:
- Communication issues
- Lack of practical programs.
Communication issues
The recently-released National Healthcare Quality and Disparities Report points out that certain racial and ethnic groups that coincide with the underserved subpopulations are the most severely uninsured. See Figure 1. (Please note that the term American Indian/Alaska Native is shortened to AI/AN, and the term Native Hawaiian/Pacific Islander is shortened to NHPI.)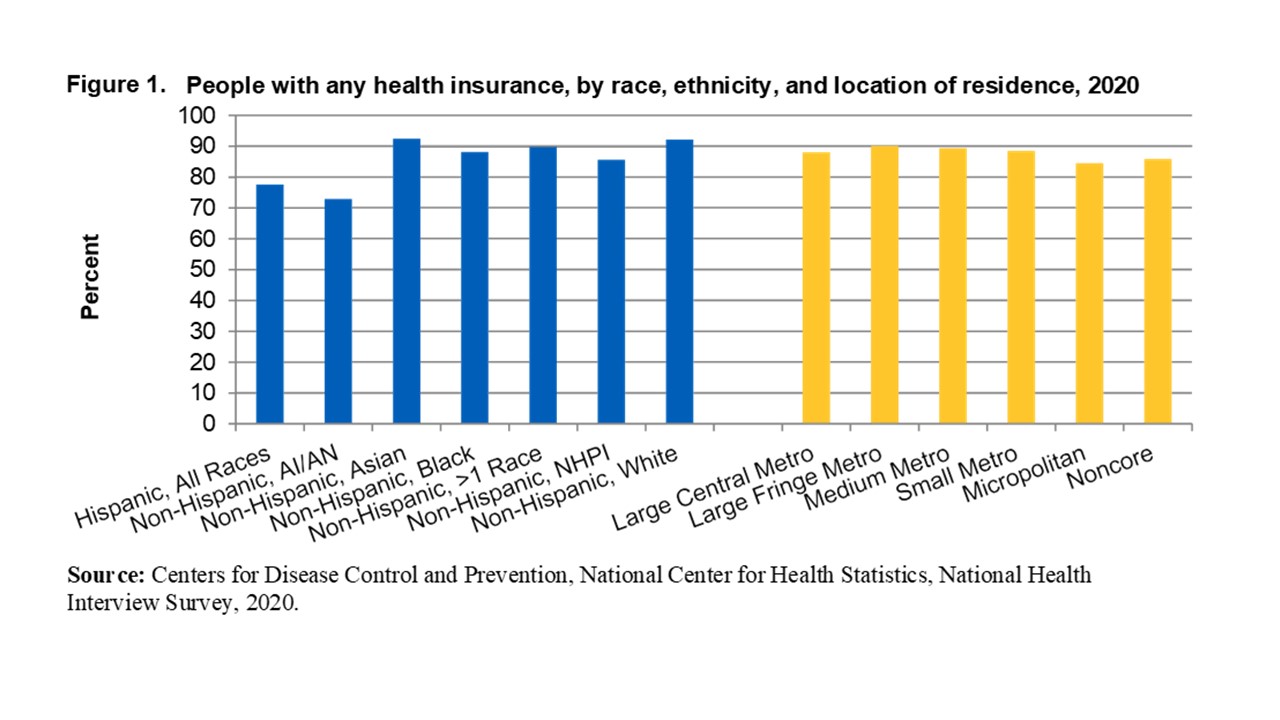 These disparities should not exist by definition, largely because of the availability of Medicare, Medicaid, and low-cost or no-cost insurance from state insurance exchanges. As the report points out, they exist largely due to communication and access issues. Many members of the underserved communities either have coverage but avoid seeking care or don’t know they’re eligible for coverage in the first place.
These disparities should not exist by definition, largely because of the availability of Medicare, Medicaid, and low-cost or no-cost insurance from state insurance exchanges. As the report points out, they exist largely due to communication and access issues. Many members of the underserved communities either have coverage but avoid seeking care or don’t know they’re eligible for coverage in the first place.
Avoiding treatment
Having coverage and avoiding care is a solvable problem, if healthcare organizations and the society in general have the will to do so. People in the underserved communities often miss planned appointments for certain medical purposes such as wellness exams, follow-up appointments, and scheduled appointments for priority services such as prenatal care and maternal wellness, causing them in the latter case to pay a high price in terms of maternal morbidity and neonatal health. (See “Lack of Practical Programs” below.) Some of this is due to language barriers, transportation issues, or unease in the interaction with healthcare personnel; but a great deal is due to a misunderstanding of the extent of their coverage, especially what remains due from the patient in the form of copayments, deductibles, etc.
Healthcare organizations can ease these problems by providing more and better-trained navigators as well as interpreters and translation services. They can build more outreach programs to the underserved to make them aware that in many cases they have little or nothing to pay for wellness services and planned care for medical purposes such as behavioral conditions, substance use treatment, chronic conditions, routine wellness care, and priority areas such as the above-mentioned prenatal care.
Not knowing about eligibility
The same potential remedy applies to lack of awareness of eligibility. Members of the underserved communities often don’t know that they’re eligible for coverage in the first place, and this leads to avoidance of treatment as well. More and better-trained health navigators supported by outreach programs can also go a long way toward alleviating this part of the problem.
Lack of practical programs
If communication with the underserved can be improved, it stands to reason that well-structured programs must be established to accommodate them. In other words, they have to have a place to go. Not enough imaginative or careful thought has been put into the development of these programs for underserved communities. Programs, personnel, and training are lacking in the areas of behavioral health, substance use treatment, dental care, prenatal/postpartum care, and more.
While the AHRQ report clearly identifies significant disparities in each of these areas for underserved communities, nowhere is the disparity more painful than in the area of prenatal care. See Figure 2.
The AHRQ data show that the level of care is well below acceptable levels for each of the four main underserved communities. This has unfortunately led to higher rates of maternal morbidity among these members of the underserved communities due to such conditions as eclampsia/preeclampsia, severe postpartum hemorrhage, venous thromboembolism, and other complications of pregnancy and childbirth.
While this is just one significant area of disparity in quality of care for the underserved, it appropriately points out the need for practical programs. Health care organizations can respond with energy and creativity by developing doula/monitrice services, transportation services, language/interpretive services, and structured prenatal and postpartum care services in tandem with the improved communication and health-navigator programs mentioned above. There’s also evidence that the provision of team-based, interprofessional, central location care centers can often lead to improved medical outcomes for underserved populations.
Information-gathering is an important first step
Clearly, different approaches will be required based on geographic, cultural, linguistic, and sociodemographic issues that pertain to your organization, but the journey always begins by gathering information. Cascade Strategies has a great deal of expertise and experience in helping healthcare companies assemble this knowledge, and we stand ready to assist you. Please tell us about your information needs at contact Cascade Strategies, and we’ll be pleased to serve your needs.